
Varikosel hakkında bilgiler
Varicocele, which can cause infertility in adult men, is also a condition we encounter in adolescents. While the frequency of varicocele is around 1% under 10 years of age, the incidence of varicocele in adolescence is 11%. The prevalence of varicocele increases gradually at the age of 13 and beyond, and at this age varicocele often does not show any symptoms. During adolescence, varicocele is mostly detected incidentally by physical examination or noticed by families. While the diagnosis of adolescent varicocele can be made by examination, ultrasonography and venography similar to adults; Today, the gold standard for the diagnosis of varicocele is physical examination. There is no need for radiological imaging methods other than examination for the diagnosis of varicocele. Measurement of testicular volumes is necessary for the necessity of varicocele treatment and for the evaluation of testicular volumes after varicocele surgery. Orchidometry is sufficient for testicular volume measurement in patients with varicocele. The accepted absolute treatment condition for varicocele detected in this period is 2 ml or more than 10% decrease in testicular volume. The aim of varicocele treatment in adolescence is to preserve fertility. The ideal varicocele surgery method should protect the testicular activities optimally, varicocele should disappear and complications should not be seen. The most common problem encountered after varicocele surgery in adolescence is postoperative hydrocele with a rate of 1 to 32%.
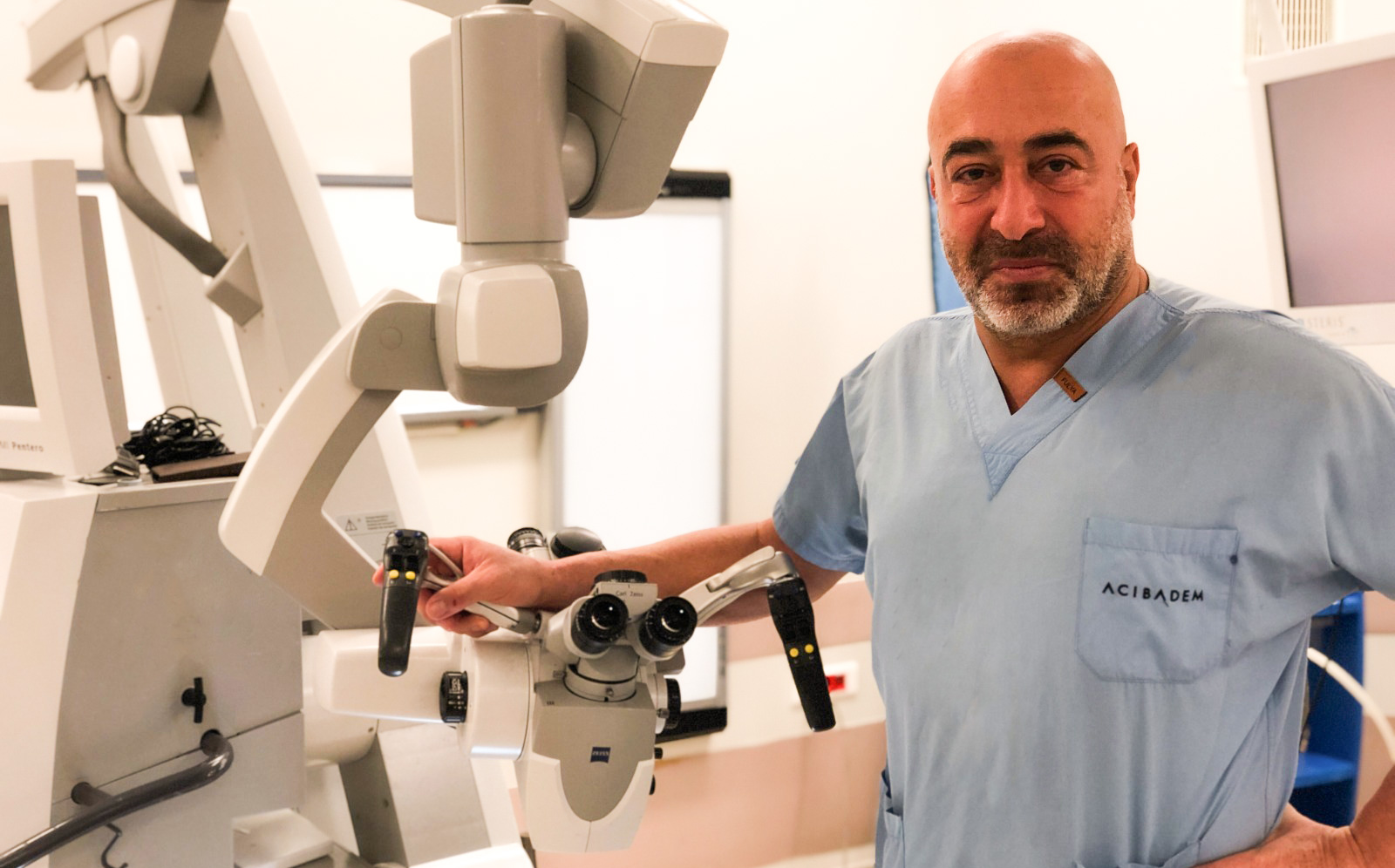
Optical magnification is necessary to reduce complications such as recurrence, arterial damage and hydrocele in pediatric and adolescent varicocele surgeries. The use of microscope in varicocele surgery reduces the complication rates to the lowest probability. While varicocele surgery can achieve normal testicular volume in those with a small testicle before varicocele surgery, in those older than 14 years of age, the consistency of the testis may improve after varicocele surgery, but there may not be sufficient improvement in the volume. Apart from testicular volumes, significant improvement can be achieved in sperm tests and hormone values after varicocele surgery in adolescent cases. The families of those who will undergo varicocele surgery should be informed about varicocele in the light of these findings. Follow-up in cases with varicocele: Children and adolescents with varicocele should be followed up annually with physical examination and volume measurement. If there is no increase in the varicocele grade detected on examination, annual follow-up and 6-month follow-up is appropriate for those with an increase in varicocele grade. In cases with varicocele and normal testicles, the measurement is made annually; Varicocele surgery should be recommended for those with volume loss. Varicocele surgery should be recommended for those with defects in the sperm test. Follow-up after adolescent varicocele surgery: In patients treated with microsurgical methods due to varicocele, an examination should be performed once a year to monitor varicocele recurrence, hydrocele, testicular consistency and volumes, and additionally, serum hormone (FSH and testosterone) tests and sperm test should be performed.
After varicocele surgery, patients should be monitored regularly. Sperm tests should be performed for 1 year after varicocele surgery or every 3 months until pregnancy is achieved. Depending on the total motile sperm count, assisted reproductive techniques such as intrauterine insemination (IUI) or in vitro fertilization (IVF) / intracytoplasmic sperm injection (ICSI) should be used in couples whose varicocele problem has been eliminated but infertility continues. Couples face infertility problem with a probability of about 20% in a period of their marriage. In this case, the problem is completely male with 20% probability, and it can be determined that there is a problem in both men and women with 40% probability. As a result, the effect of the male factor on the infertility problem of couples can reach up to 60%. The causes of male infertility can usually be revealed by sperm analysis and examination; In some cases, further investigations are required. Infertility does not have a clear distinction like black and white, and is usually seen in gray tones; that is, the person is mostly not completely sterile and the probability of having a child is partially reduced. In this case, the aim is to optimize the person and ensure that the couple has a child as a result of the treatments. It is a very common mistake to start infertility treatment for women without examining the man by a Urologist-Andrologist and evaluating the spermiogram performed in a specialist laboratory. It should not be forgotten that male infertility may be a symptom of an underlying and life-threatening serious disease.
The testicles are formed at the same level as the kidneys during development in the mother's womb and move down over time. During this movement, they pass out of the abdomen by passing through the inguinal canal and generally settle in the bag before birth. During this migration, the testicles carry their veins with them; therefore, the main vein of the left testis is poured directly into the vein of the left kidney. Varicose veins are common because there are no muscles around these veins, which form an upright column when we stand, like the veins in the legs and pump them by compressing them. The valves that form the check-valve mechanism in the veins, called veins, become insufficient with the enlargement of the vein diameter and cannot prevent reverse flow. In this case, in situations that increase intra-abdominal pressure such as taking a deep breath or lifting a weight, blood flows back to the testis, increasing the pressure at the testicular outlet, slowing the blood flow in the testis and affecting its functions.
The diagnosis of varicocele should be made by hand examination. I do not perform surgery in cases where it is said that there is varicocele only with Doppler ultrasound, which I did not detect in my hand examination; Surgery is not beneficial in these patients. The examination is carried out standing up and in a non-cold environment. Grade 3 varicocele is diagnosed if the varicose veins can be seen with the eye, Grade 2 varicocele if the veins are found to be convoluted on hand examination or become convoluted with straining, Grade 1 varicocele is diagnosed if it is felt that the vein is filled from top to bottom, albeit a little late, only by straining. The negative effect of varicocele does not always show parallelism with its degree. Varicocele shows its effects by increasing over the years, even if it is the first child, it may not be the second child. Varicocele begins in adolescence, does not constitute an emergency, surgery is recommended within a few months if necessary.
Varicocele does not directly cause erectile dysfunction in men, but over time, varicocele can affect the testicles and reduce the male hormone testosterone to some extent. Decreased testosterone amounts due to varicocele can also be seen together with decreased sexual desire and decreased sexual performance. Varicocele is present in 15-20% of all men and 40% of those with infertility problems. As a result of varicocele, a- number, b- motility c- morphology (structure) d- vitality parameters may be impaired in sperm; d- DNA Fragmentation Index (DFI) may increase. As a result of the increase in DFI (increase in the rate of fragmentation in sperm DNA), the capacity of the sperm to fertilize the egg decreases and the probability of early miscarriage increases even if fertilization occurs. In addition, patients with varicocele may experience pain and decrease in testosterone, which is the male hormone, over time. For these reasons, the first treatment to be applied in a man with varicocele is microsurgical varicocele surgery; these couples should not be directed to assisted reproductive techniques such as ICSI (in vitro fertilization) before varicocele surgery.
The used dirty blood is removed from the testis by 3 ways.
The purpose of all varicocele surgeries is to perform the above-mentioned procedures and to protect the lymphatic channels and arteries of the testis while doing this. However, in surgeries that do not use microsurgery Lymphatic channels and testicular artery can be connected unintentionally because they cannot be seen b- One or more of the internal spermatic vein branches can be bypassed easily. For this reason, in non-microsurgical varicocele surgeries; The probability of varicocele recurrence can be up to 40%; In this case, the operation is unsuccessful and microsurgical correction surgery is performed. The accumulation of water around the testis, called hydrocele, can be seen in up to 20% and may require additional surgery. As a result of the ligation of the testicular artery, there is a possibility of loss of the organ in 5% of the operations. Considering all these complications, varicocele surgery should be microsurgery. Microsurgical varicocele surgery is not a simple operation; The probability of varicocele recurrence is less than 1%. The incidence of hydrocele is 0% because the lymph channels are preserved. The risk of ligation is 0% since the arteries are protected by being visible.


